When employees travel for work for a few months at a time, it can be tempting to file “health cover” under travel administration. In practice, it often sits at the intersection of global mobility, duty of care and the employee experience you’re trying to protect. For HR, the aim isn’t to buy the most cover — it’s to build a benefits approach that works across countries, time zones and real-world healthcare systems.
Short-term international assignments can make commercial sense — you can deploy expertise quickly without the complexity of a long-term relocation. But from a people perspective, “a few months” is long enough for medical needs to arise: an accident, a flare-up of a chronic condition, mental health support, or simply the need to access care in an unfamiliar system.
HR leaders are often balancing four pressures at once: retaining key talent, meeting duty-of-care expectations, keeping benefits equitable, and avoiding unintended compliance issues across jurisdictions. The challenge is that domestic health plans and standard travel insurance aren’t always designed for the middle ground between a “business trip” and an “expat relocation”.
This guide explains what typically changes when you move from domestic benefits to international cover, how to think about value (not just premium), and how to design a practical, defensible and employee-friendly approach for EU and APAC assignments — without making promises your benefits can’t deliver.
- Short assignments still create real healthcare demand — and friction (language, billing, access) can be as costly as treatment.
- Domestic plans rarely translate neatly into cross-border care; the gaps are often administration and access, not “headline cover”.
- ROI is contextual: value can show up in retention risk, downtime, claims friction and the cost of delayed care — not just medical spend.
- Group IPMI can be structured for mobility (e.g., defined assignment groups, area of cover, networks and direct billing), but eligibility and terms vary by policy.
- Compliance is multi-layered: employment law, social security/posted worker rules, insurance admissibility, and health data privacy (especially in the EU).
- Design starts with your mobility reality: destinations, duration, employee profiles, and what “good” looks like operationally (claims, support, communications).
- A broker’s value is governance plus execution: aligning cover to mobility policy, documentation and ongoing support — not naming “the best insurer”.
Why health benefits matter in global mobility
Global mobility is no longer limited to multi-year expat packages. Many organisations now rely on short-term assignments, project deployments and frequent travel to put skills where they’re needed. Recent mobility benchmarking continues to show employers using a mix of long- and short-term moves — and revisiting policies as risk, cost and compliance pressures increase.[1][2]
For employees, “a few months abroad” quickly changes three things: access to care, confidence in support, and the sense of how well the employer has planned for the realities of being away from home. These factors can influence engagement and retention. In WTW’s 2024 Global Benefits Attitudes Survey, employees across regions increasingly report that benefits are an important factor when choosing an employer, with notable increases since earlier survey waves (including in EMEA and Asia Pacific).[3]
Short-term assignments sit in a “grey zone”
Short assignments often fall between categories: travel insurance may be geared towards emergencies and trip disruption, while domestic health plans are typically designed for care delivered within a single system. If your mobility policy expects employees to work effectively abroad, it helps to treat healthcare access as part of operational readiness — not a perk.
Benefits can support retention when they reduce uncertainty and make life abroad workable. Employee perceptions of benefits have become a stronger factor in employment decisions over time, according to global benefits-attitudes research.[3]
A structured travel risk management approach (e.g., aligned with ISO 31030 guidance) treats health incidents as part of travel risk, alongside security and operational disruption.[4]
A straightforward access or claims issue can quickly become project downtime — especially when employees don’t know where to go, how to pay, or how to obtain pre-authorisation in another country.
What “good” looks like for HR
For short assignments, HR outcomes tend to be practical:
- Fast access to appropriate care (not just emergency cover).
- Low-friction payment (where possible) through networks and direct billing, rather than high out-of-pocket costs.
- Clear employee guidance on what to do before travel, during the assignment, and in an emergency.
- Country-aware governance (employment law, social security rules, and health data privacy).
- Consistency across destinations without over-engineering benefits for every single country.
Global mobility is your organisation’s framework for moving employees across borders (short-term and long-term). International assignments can include project deployments for a few months, secondments, and longer relocations. Group IPMI refers to International Private Medical Insurance arranged on a group basis — typically designed for cross-border care needs and international access (policy terms vary).
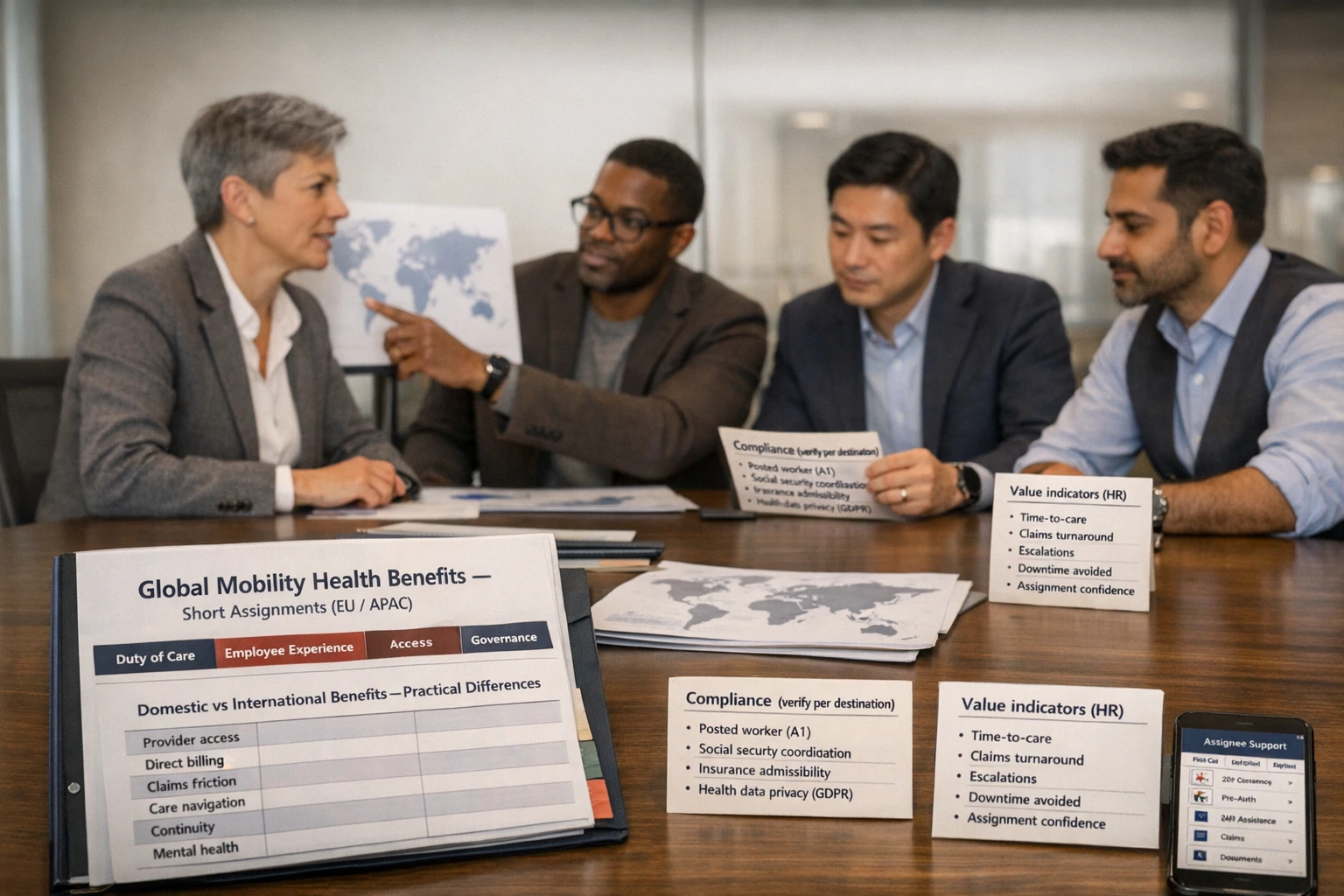
Differences between domestic and international benefits
When HR compares domestic and international health benefits, the obvious differences are “territory” and “cost”. In practice, what employees notice most is often: how care is accessed, how it is paid for, and how issues are resolved across borders.
Domestic plans can be strong — but are “domestic-first” by design
Domestic plans are typically built around one healthcare ecosystem: a local provider network, local billing norms, and local regulatory expectations. Once an employee is abroad for months, the same plan may still reimburse eligible treatment — but the day-to-day experience can change significantly (additional paperwork, translation, longer reimbursement timescales, limits on out-of-area treatment, or the need to pay providers upfront).
International cover is often about access and navigation
International medical cover (including group IPMI structures) is usually built for cross-border use: multilingual assistance, international provider networks, and clearer processes for paying providers. That doesn’t mean it is “better” in every context — it means it is designed to solve a different problem.
| Practical factor (HR-friendly) | Domestic plan + travel add-ons (typical) | International cover / group IPMI (typical) | What to check (your situation) |
|---|---|---|---|
| Where cover applies | Primarily home country; limited out-of-area reimbursement may apply. | Designed for multiple countries; area of cover is often selectable (e.g., worldwide vs excluding certain high-cost markets). | Assignment countries, trip frequency, and whether commuting between countries is expected. |
| Access to providers | Strong domestic network; overseas access may be “any provider” but with reimbursement and administration friction. | International networks may support quicker access and clearer pathways for eligible treatment. | Network presence in key EU/APAC cities; how employees find in-network care. |
| Direct billing / cashless care | Often limited abroad; employees may need to pay upfront and claim back. | May offer direct billing for eligible treatment at participating providers, reducing upfront costs (depends on network and treatment type). | Which services are typically cashless; emergency vs routine vs specialist care. |
| Claims administration (time + complexity) | Claims processes optimised for domestic care; overseas claims often require extra documentation. | Often designed for international claims, with multilingual support and established cross-border processes. | Who supports employees day-to-day; expected claim turnaround times; documentation requirements. |
| Emergency assistance & evacuation | Travel insurance may provide emergency assistance; domestic plans often do not. | International medical policies often include assistance services; terms vary by policy. | Definition of “medical necessity”; pre-authorisation process; what’s included vs excluded. |
| Continuity of care | Continuity may be strong at home; overseas care can be more fragmented. | May support continuity across multiple locations (subject to policy terms and provider availability). | Employees with chronic conditions; medication access; follow-ups across borders. |
| Mental health support | Domestic cover may apply at home; overseas access can be inconsistent. | Some international plans include mental health benefits and care navigation; scope varies. | Access model (in-person vs telehealth), session limits (if any), and local availability. |
| Employee experience | Can feel “DIY” abroad: finding care, paying, and claiming. | Often designed to reduce friction via networks, guidance and support. | What employees are told before travel; where they go for help; escalation routes. |
| Employer governance | May be simpler administratively, but gaps can emerge in cross-border compliance. | May align better with mobility governance, but still requires country-by-country checks. | Employment status, posted worker obligations, social security, and data privacy. |
Most assignment issues aren’t about whether a treatment is “covered in principle”. They’re about whether the employee can access care quickly, pay without financial stress, and get real-time support when something goes wrong.
Domestic vs international isn’t always a binary choice
Many employers use a layered approach for short assignments:
- Domestic plan remains the core benefit at home.
- Travel risk + emergency assistance addresses trip-related risks and urgent incidents.
- International medical cover (sometimes via group IPMI structures) supports access, networks and claims while employees are abroad for months.
The right structure depends on your destinations, assignment duration, employee profile, and the local rules that apply to the assignment.
Cost vs value: the ROI of employee wellbeing
HR teams often face the same question from finance: “Is international health cover worth it for short assignments?” A helpful answer separates premium from overall value, and uses an ROI lens that reflects your real-world risks.
Start with what’s driving cost pressure
Healthcare costs have been rising across markets, and employers increasingly feel that pressure in insured schemes at renewal. For example, WTW’s global medical trend research has reported sustained double-digit medical trend projections in some markets, with regional variation — including Asia Pacific and Europe.[5]
That doesn’t mean you should “buy more insurance”. It means you need clarity on what you’re buying: risk transfer (financial protection), access (care pathways), and operational resilience (less disruption when employees are overseas).
ROI: what the research suggests (and what it doesn’t)
Evidence on ROI in wellbeing and employer-sponsored health support is mixed — partly because programmes vary widely in design, participation and measurement. Some studies and modelling suggest meaningful returns, while more rigorous evaluations have sometimes shown limited short-term impact on medical spend.
Deloitte’s “case for investment” research on workplace mental health reported an average return estimate of around £5 for each £1 spent (with wide variation by intervention type and context).[6]
A 2025 meta-analysis examining enhanced behavioural health services reported a pooled ROI multiple of 2.3 (with variation across employers), and noted that outcomes depend on underlying assumptions and study design.[7]
A randomised evaluation of a workplace wellness programme (Song et al., JAMA) found improvements in some self-reported behaviours but no significant differences in clinical measures, healthcare spending or employment outcomes after 18 months.[8]
This doesn’t mean “wellbeing never works”. It means design, targeting, timeframe and measurement matter — and savings are not guaranteed.
Global travel risk guidance (e.g., in the ISO 31030 context) frames health incidents as business risk that can affect continuity, legal exposure and traveller confidence — outcomes that don’t always show up in medical claims analysis.[4]
ROI figures are highly sensitive to assumptions: who participates, baseline health risks, local healthcare costs, what counts as “return”, and the time horizon. Even where research reports positive ROI, that does not mean your programme will deliver the same result. Use ROI as a decision-making tool — not a promise.
What HR can measure for short assignments
For international assignments lasting a few months, HR can build an ROI narrative around operational and people outcomes you can actually track:
- Project downtime avoided: time lost due to delayed access to care, administration issues, or treatment disruption.
- Claims friction: volume of escalations, reimbursement delays, employee out-of-pocket exposure (and the time HR spends resolving issues).
- Mobility participation: whether employees accept assignments, and how confident they feel travelling.
- Retention risk: where benefits experience forms part of the employee value proposition; benefits have become more important in joining decisions in global survey data.[3]
A reality check: the cost of ill health is not abstract
Public reporting on work-related ill health continues to highlight the scale of mental health impacts on work. For example, the UK HSE’s annual statistics (Great Britain) reported substantial working days lost linked to work-related ill health and a large number of workers reporting stress, depression or anxiety attributable to work (figures vary by year and jurisdiction).[9]
This is not a reason to “sell” more insurance — it’s a reminder that employer health and wellbeing decisions sit alongside productivity, absence and the employee experience.
Translate “investment” into a CFO-friendly narrative
A simple internal model:
- Define the assignment population (who travels, where, for how long).
- Define the risks you are reducing (medical costs, access disruption, duty-of-care exposure, retention friction).
- Select 3–5 measurable indicators (claims turnaround, escalations, time-to-care, assignment acceptance, employee feedback).
- Track outcomes across renewal cycles to see what improves and where benefits design needs refinement.
Key features of group IPMI
Group IPMI (International Private Medical Insurance) is typically designed for cross-border healthcare access and administration. It’s most often associated with long-term expats, but some employers use group IPMI (or international medical arrangements with similar features) to support frequent travellers and short-term assignees — depending on eligibility rules and policy design.
What tends to matter most for “a few months abroad”
A key practical difference is how employees identify appropriate care abroad. International networks can reduce the “where do I go?” problem, particularly in unfamiliar systems.
Direct billing means the insurer (or assistance partner) pays the provider directly for eligible treatment, rather than reimbursing the employee later. Availability depends on the provider, country and type of care.
Cross-border support (multilingual helplines, guidance on facilities, and escalation routes) can make the difference between “covered on paper” and “usable in practice”.
Many international medical solutions include, or coordinate, emergency assistance services. The scope, triggers and authorisation steps vary by policy — these details are worth confirming before employees travel.
Common design levers (what HR can often choose)
Without implying guaranteed terms, these are the levers employers typically consider when evaluating international cover:
- Territory / area of cover: worldwide, or worldwide excluding certain high-cost markets (structure depends on insurer and plan).
- Eligibility: who is covered (assignees only, travellers above a duration threshold, accompanying family members).
- Benefit scope: inpatient vs inpatient + outpatient; mental health, rehabilitation and preventive services (definitions vary).
- Network model: how provider access works in key cities and countries.
- Cost sharing: excess/deductibles, co-insurance/co-payments, and how these apply across borders.
- Operational model: pre-authorisation rules, claims submission channels, and employer reporting.
Some group medical arrangements use EOI / evidence of insurability for certain employee groups or benefit levels. This is where the insurer requests health information to assess eligibility for cover. Whether EOI applies, and when, is policy-specific — so it’s worth clarifying early for mobility populations.
How group IPMI intersects with flexible benefits
Some employers use flexible benefits to offer “mobility-ready” health cover as an option for eligible employees. If you take this route, clarity is essential: employees need to understand when cover applies (e.g., while on assignment), how to access care, and what to do in an emergency.
EU & APAC note: In some markets, employers may face constraints on how private medical cover can be offered, or how it sits alongside local systems. Treat plan design as a joint HR + broker exercise, with local legal/tax input where needed.
Compliance across jurisdictions
Compliance is where many apparently “simple” mobility benefits strategies become complex. For short assignments, you’re rarely dealing with a single rule set — you may be navigating employment law, social security, insurance rules and privacy obligations at the same time.
1) Employment and mobility status: what is the assignment in legal terms?
In the EU, some assignments may fall under “posted worker” frameworks depending on how the employee is sent and what work they perform. The European Commission describes posted workers as employees sent by their employer to provide a service in another EU country on a temporary basis.[10]
That classification can affect which employment protections apply, what documentation is needed, and how benefits are treated. It doesn’t automatically dictate your insurance solution — but it should be reflected in your compliance checklist.
2) Social security and “where are contributions paid?”
Cross-border assignments can raise social security coordination issues. In the EU/EEA/Switzerland, documentation such as the A1 certificate is commonly used to evidence which country’s social security legislation applies when an employee works temporarily in another country (where eligible and applicable).[11]
Social security coordination is not the same as private medical insurance. You may need both: a compliant position on social security and a practical benefits solution for healthcare access while abroad.
3) Health data privacy (EU focus)
Benefits administration can involve sensitive personal data — particularly health information used for enrolment, claims support, reasonable adjustments, or wellbeing services. EU guidance notes that certain categories of personal data (including health data) require additional protection and an appropriate legal basis under GDPR.[12]
Practical implications for HR include:
- Data minimisation: collect only what you need for administration and support.
- Role clarity: understand which parties are controllers/processors, and what contracts are required.
- Cross-border transfers: if vendors process data outside the EU/UK, appropriate transfer safeguards may be required.
- Employee communications: privacy notices and a clear explanation of what is processed and why.
This guide focuses on EU and APAC mobility. For MENA assignments, requirements and market practice can differ materially by country; in some cases, you may want a specialist broker with strong local capability to validate requirements and implementation.
4) Insurance admissibility and local requirements
Some countries have mandatory insurance rules, local registration requirements, or constraints on how private medical insurance interacts with local systems. Even for “a few months”, it’s safer to treat this as something to verify, rather than assume.
A useful way to approach this is to separate:
- What is legally required (employment, social security, mandatory insurance rules).
- What is operationally necessary (care access, direct billing, emergency support, employee clarity).
- What is culturally expected (how healthcare is accessed and paid for in that country).
Steps to design a benefits strategy
A strong international benefits strategy for short assignments is built much like a policy: clear scope, clear governance and clear instructions for employees. Below is a practical sequence that often works well for EU and APAC programmes.
Step 1: Map your mobility reality
Segment by assignment duration (e.g., 4–12 weeks, 3–6 months), role criticality, and whether family members accompany.
Prioritise destinations where language barriers, provider access, or billing norms make “reimburse later” unrealistic.
Consider workforce demographics, job hazards, and the likelihood of mental health needs during high-pressure projects abroad.
Step 2: Choose your benefits architecture
Most HR teams choose between three approaches (or a hybrid):
- Domestic-first + reimbursement: workable for low-friction destinations and shorter durations, but can create cashflow issues for employees and add administration.
- Travel + emergency focus: appropriate for true business travel, but may not support routine care over several months.
- International medical layer: supports access and day-to-day usability for assignment populations; requires careful design and compliance checks.
Step 3: Put governance in place (so benefits remain controllable)
Governance is where you protect both employees and the business:
- Eligibility rules: who qualifies for which cover, triggered by duration/destination/role.
- Approvals: how assignments are approved and recorded (mobility + HR + risk).
- Escalation routes: what happens when an employee can’t access care or hits a claims issue.
- Vendor management: service levels, reporting and renewal discipline.
Checklist: design considerations (use this before you buy)
- Benefits scope: inpatient/outpatient balance; emergency and evacuation support; mental health access; approach to preventive and chronic care (confirm policy definitions).
- Territory: EU + APAC destinations covered; how “temporary travel” and “assignment residence” are defined; any country restrictions.
- Network & access: in-network presence in key cities; how employees find providers; language support.
- Direct billing: where cashless access is available; when employees pay upfront; reimbursement timescales.
- Governance: eligibility rules; approvals; escalation; vendor service levels; renewal cadence.
- Communications: pre-travel briefing; “what to do” guide; emergency contacts; claims steps; FAQs in plain English.
- Compliance: posted worker considerations (EU); social security documentation where applicable;[10][11] insurance admissibility; mandatory local rules (verify per destination).
- Data privacy: health data handling; vendor contracts; cross-border transfers; employee privacy notices and data minimisation.[12]
- Claims & renewals: reporting you receive; claims escalation processes; renewal strategy and cost-management levers.
Step 4: Implement it like an employee product
Even a well-designed plan can fall down if employees don’t know how to use it. Treat rollout as you would any critical people process:
- A one-page “how to use it” guide (before travel, during the assignment, and in an emergency).
- Manager enablement so project leads know what support looks like.
- A feedback loop after the first cohort travels: what broke, what confused people, what delayed access to care.
What to ask your broker/insurer (HR-focused)
- How does the policy define travel vs residence/assignment, and what duration triggers different terms?
- Which EU/APAC cities have strong network coverage and direct billing for outpatient and inpatient treatment?
- What are the pre-authorisation requirements, and how quickly can approvals be obtained across time zones?
- How are claims escalations handled, and what reporting can HR expect (without accessing sensitive health data unnecessarily)?
- Does the arrangement involve EOI for any employee groups, and what is the process?
- What data is processed, where, and what privacy and cross-border transfer safeguards are in place?
- At renewal, what levers exist to manage cost without undermining employee access?
How a broker helps employers
In international health benefits, a broker’s role isn’t to claim there is a single “best” insurer. The value is in shaping market options into a benefits solution that matches your mobility policy, risk appetite and operational reality — and then keeping it workable over time.
1) We translate mobility policy into benefits architecture
Short-term assignments often include multiple patterns: project travel, rotating deployments, and multi-country trips. We help you turn those patterns into clear eligibility rules and a coverage structure so employees know what applies, and when.
2) We stress-test access and administration (not just benefit tables)
The day-to-day experience matters: direct billing availability, provider access in key cities, and escalation workflows. We focus on “can the employee use this in practice?” because that’s where friction — and dissatisfaction — tends to build.
3) We support compliance coordination across jurisdictions
For EU mobility, this can include helping HR identify where posted worker and social security coordination questions may arise, and ensuring you know what to verify.[10][11] On privacy, we help you think through health data handling and vendor governance in a way that aligns with GDPR expectations and good practice.[12]
4) We help you build an ROI narrative that is honest and defensible
ROI claims need careful handling — wellbeing outcomes depend on context and programme design. We can help you choose metrics that match your assignment reality and interpret research responsibly: for example, Deloitte’s modelling suggests average positive returns for mental health interventions with wide variation,[6] while controlled evaluations of some wellness programmes show limited short-term effects on medical spending.[8]
5) We stay involved after placement
International cover is operational. We support onboarding communications, claims escalation routes, and renewal planning so you don’t “buy a policy” and then rebuild the same solution every year.
If your mobility programme becomes easier to run, employee confidence improves, and claims/administration friction reduces over time, you’re seeing value. If HR still spends disproportionate time firefighting access and claims issues, the strategy likely needs adjustment — regardless of which insurer is on the ID card.
If you’re reviewing global employee health benefits for short-term EU and APAC assignments, we can help you structure options, clarify compliance checks, and build a practical rollout plan.
Further reading: Choosing the Right Insurer for International Health Insurance | IPMI Abroad: The Guide to Getting Health Cover Right Before You Move